Endometriosis: Causes, Symptoms, Diagnosis, and Treatment
Endometriosis: Causes, Symptoms, Diagnosis & Treatment
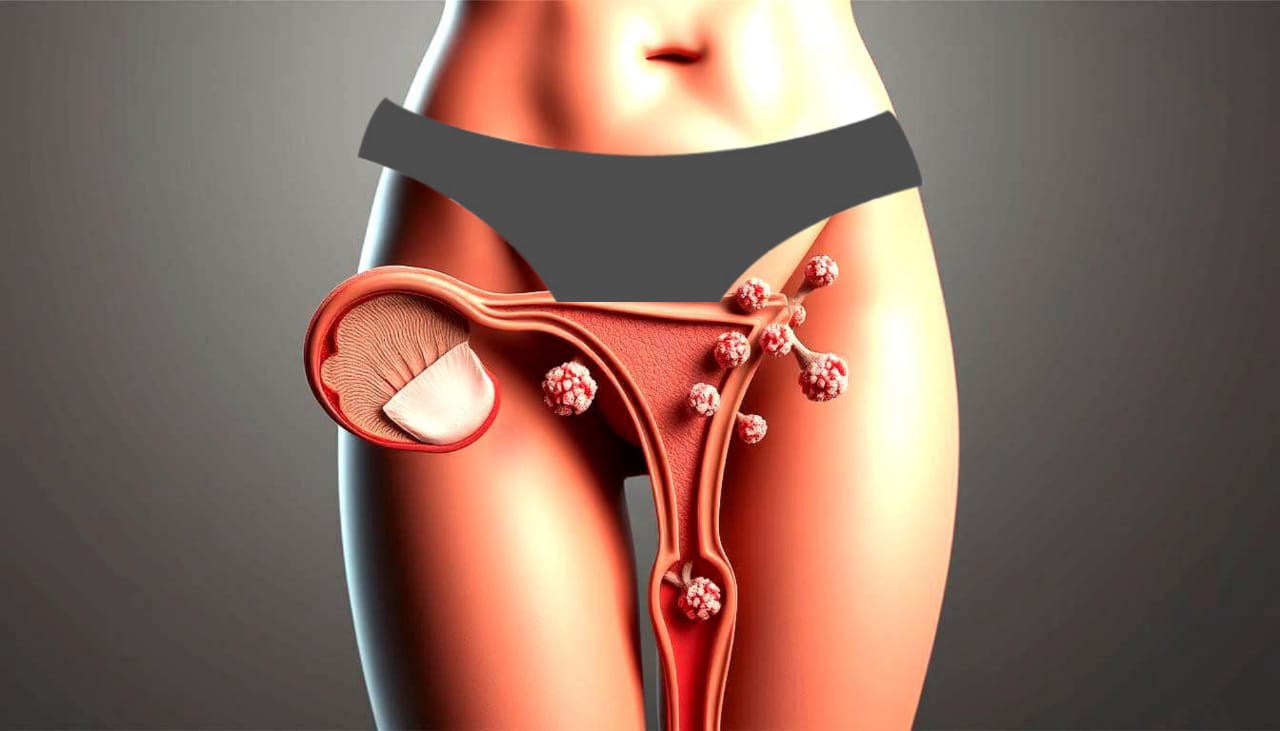
Endometriosis affects about 10% of women of childbearing age. This means around 176 million women worldwide are impacted. It causes tissue like the lining of the uterus to grow outside the uterus. This often leads to severe pelvic pain, felt by 70-90% of those with endometriosis.
This condition not only hurts physically but also affects female reproductive health. 30-50% of women with endometriosis struggle to get pregnant. It’s a big challenge for their health and well-being.
It’s important to know about the causes, symptoms, diagnosis, and treatment of endometriosis. This knowledge helps those affected and their doctors. Even though it’s usually diagnosed at 27 years old, symptoms can start in teens as young as 15.
This article is based on the latest research and expert advice. It aims to offer detailed support and information for dealing with this tough condition.

What is Endometriosis?
Endometriosis is a condition where tissue like the uterus lining grows outside the uterus. This tissue often appears on organs like the ovaries and fallopian tubes. Each month, this tissue reacts to hormones, causing inflammation and severe pain.
About 2 to 10 percent of American women aged 25 to 40 have endometriosis. It affects up to 10% of women aged 15 to 44. Studies show that 24% to 50% of women with infertility issues have endometriosis.
Endometrial tissue outside its usual place causes severe symptoms. People with this condition often have chronic pelvic pain. This pain can get worse during menstruation, sex, and even when they go to the bathroom.
Endometriosis can start at the first period and last until menopause. It’s more common in those with early menstruation, short cycles, or heavy bleeding. Getting a diagnosis can take 4 to 11 years, making treatment harder to find.
Understanding the Causes of Endometriosis
The exact Causes of Endometriosis are still a mystery. Researchers look at several possible reasons. One idea is that menstrual blood flows back into the pelvic area. This can cause endometrial cells to grow outside the uterus.
Genetics also play a big role. If your family has endometriosis, you’re more likely to get it. Scientists have found certain genes that might be linked to the condition.
Hormones are another key factor. Estrogen helps endometrial tissue grow, which can worsen symptoms. Studies show that hormone therapy can help manage these symptoms.
Immune system problems might also cause endometriosis. Sometimes, the body doesn’t recognize endometrial tissue outside the uterus. The way different cells turn into endometrial-like tissue is also a mystery. Figuring out these causes is important for finding better treatments.
| Factor | Description |
|---|---|
| Retrograde Menstruation | Menstrual blood flows backward into the pelvic cavity, allowing endometrial cells to grow outside the uterus. |
| Genetic Factors | Family history increases the likelihood of developing endometriosis, with certain genetic markers being identified. |
| Hormonal Factors | Estrogen plays a significant role in the growth of endometrial tissue, influencing the severity of symptoms. |
| Immune System Disorders | Issues with the immune response may lead to poor recognition of endometrial tissue outside the uterus. |
| Cell Transformation | The transformation of various cells into endometrial-like tissues contributes to the complexity of endometriosis. |
Endometriosis: Causes, Symptoms, Diagnosis, and Treatment
Endometriosis affects about 200 million women worldwide. In the U.S., it impacts one in 10 women. It can start as early as pre-teen years, often before a woman’s first period. Most women experience their worst symptoms in their 20s and 30s, leading to a lot of discomfort and health issues.
It’s important to know the Symptoms of endometriosis. But, it takes an average of 10 years to get a correct diagnosis in the U.S. Many women are misdiagnosed, often thought to have IBS, appendicitis, or pelvic inflammatory disease. Only a small fraction of women with retrograde menstruation are diagnosed with symptomatic endometriosis.
Doctors use many tests to diagnose endometriosis. They use advanced ultrasounds and MRIs because regular ultrasounds might miss the signs. They talk about symptoms and do tests to confirm the disease.
For Treatment Options, the best method is a minimally invasive surgery to remove deep endometriosis. Surgery can help with severe symptoms, but a hysterectomy doesn’t always cure it. Many women still have pain after surgery. Hormonal treatments and lifestyle changes can help manage symptoms better.
| Aspect | Details |
|---|---|
| Prevalence | Affects 200 million women globally; 10% of reproductive-aged women in the U.S. |
| Typical Onset | Can start in pre-teen years, with severe symptoms often in 20s and 30s |
| Diagnosis Lag Time | Average of 10 years from symptom onset to receiving diagnosis |
| Common Misdiagnoses | IBS, appendicitis, ovarian cancer, colon cancer, pelvic inflammatory disease |
| Surgical Approach | Minimally invasive laparoscopic excision deemed most effective |
| Post-Surgery Experience | Many women still experience pain, hysterectomy is not a definitive cure |
Identifying the Symptoms of Endometriosis
It’s important to know the symptoms of endometriosis early. This condition can show up in different ways. Pelvic pain is a big sign, and it can happen all month, not just during your period.
Pelvic Pain and Its Severity
Pelvic pain is a key symptom of endometriosis. It often happens during your period but can occur at any time. The pain can be mild or very severe, making it hard to do everyday things.
Some people feel such intense cramps that they can’t go about their day. This pain can also be linked to heavy bleeding, making it hard to change pads or tampons often. This can be both embarrassing and uncomfortable.
click here know What is Cancer? | Easy Guide for Everyone
Other Common Symptoms
Endometriosis also brings other symptoms, including:
- Pain during bowel movements or urination
- Pain during or after sexual intercourse
- Heavy periods (menorrhagia)
- Extreme fatigue
- Gastrointestinal issues like bloating, diarrhea, and constipation
- Infertility, affecting nearly 40% of those diagnosed with endometriosis
People with endometriosis may also feel more anxious or sad, especially if they’re having trouble getting pregnant. Even after menopause, some symptoms can still be present. But, many women find relief after menopause.
Knowing the many symptoms of endometriosis is crucial. It helps those affected get the right medical help and treatment.
Diagnosis of Endometriosis
Diagnosing endometriosis starts with a detailed talk with a healthcare provider. They discuss symptoms and medical history. This helps understand the patient’s experiences and look for signs of endometriosis. Finding the right diagnosis can take several years.
Initial Consultation and Symptom Discussion
At the first meeting, patients often talk about chronic pelvic pain, irregular periods, and pain during sex. A pelvic exam might be done. This helps narrow down possible causes and decide if more tests are needed.
Diagnostic Procedures
Laparoscopic surgery is key to diagnosing endometriosis. It lets doctors see inside the pelvic area and take tissue samples. Ultrasounds and MRIs help too. But, it can take 7 to 10 years to get a diagnosis after symptoms start. Early diagnosis through laparoscopy helps plan the right treatment.
| Diagnostic Method | Purpose | Details |
|---|---|---|
| Initial Consultation | Evaluate symptoms | Discussion about pelvic pain and medical history |
| Pelvic Exam | Physical assessment | Check for abnormalities and tenderness |
| Imaging Tests | Visualize pelvic structures | Ultrasounds or MRIs to assess potential issues |
| Laparoscopy | Confirm diagnosis | Surgical inspection and possible biopsy of tissue |
Risk Factors for Developing Endometriosis
Endometriosis affects over 11% of menstruating women in the United States between the ages of 15 to 44. Several factors increase the risk of developing this condition. Family History is a key factor, with a 7 to 10 times higher risk for those with a family history of endometriosis. Knowing these risk factors can help in early diagnosis and management.
Menstrual Cycle Characteristics also play a role. Women who start menstruating before 12 are more likely to develop endometriosis. Longer periods, lasting seven days or more, also increase the risk. Conditions that lead to retrograde menstrual flow, such as high estrogen levels or uterine growths, are linked to a higher risk.
Pregnancy can protect against endometriosis by reducing menstrual cycles. A weak immune system that fails to recognize misplaced endometrial tissue is another risk factor. Abdominal surgeries can also lead to misplaced endometrial tissue, sometimes causing endometriosis.
Women who have never given birth face a higher risk. High estrogen levels, which can cause heavy menstrual bleeding, are another risk factor. Medical conditions that prevent normal menstrual blood flow and a history of pelvic infections and uterine abnormalities also increase the risk.
| Risk Factor | Details |
|---|---|
| Family History | Increases risk 7 to 10 times. |
| Early Menstruation | Starting periods before age 12 increases risk. |
| Menstrual Cycle Length | Periods lasting seven days or longer increase susceptibility. |
| Pregnancy | Reduces number of menstrual cycles; protective factor. |
| Uterine Issues | Conditions that cause retrograde flow or abnormal structure increase risk. |
| Weak Immune System | May fail to recognize misplaced endometrial tissue. |
| Abdominal Surgeries | Might misplace endometrial tissue. |
| Heavy Menstrual Bleeding | Associated with high estrogen levels and increased risk. |
Complications Related to Endometriosis
Endometriosis is a complex condition that affects women’s health. It can lead to various complications. One major issue is its impact on fertility. Understanding these complications is key to managing the condition and improving quality of life.
Impact on Fertility
Infertility is a big concern for women with endometriosis. It’s estimated that 30-50% of women with this condition face challenges when trying to conceive. The endometrial-like tissue can block the path of sperm and eggs, making it hard to conceive naturally.
The link between endometriosis and infertility is strong. This shows why early diagnosis and treatment are crucial for affected women.
Potential Long-Term Health Issues
Endometriosis can cause chronic pain and other problems. About 10-20% of people with endometriosis have issues with their bowels and bladders. Chronic pain affects around 40% of women with endometriosis, leading to emotional distress.
While rare, severe complications like lung or diaphragm involvement can happen. This highlights the need for comprehensive management strategies for this condition.
Treatment Options for Endometriosis
Dealing with endometriosis means finding a treatment that fits you best. At first, doctors often try nonsurgical methods to ease symptoms and improve life quality. For many, Hormone Therapy is a key option. It helps control menstrual cycles, lowers endometrial tissue activity, and eases pain.
Nonsurgical Treatments
Non-surgical treatments for endometriosis include medicines and lifestyle changes. Endometriosis Treatment might include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief.
- Hormonal medications like birth control pills, patches, or hormonal IUDs that help in reducing menstrual pain.
- Gonadotropin-releasing hormone (GnRH) agonists, which can temporarily induce menopause to relieve symptoms.
These treatments can help reduce chronic pain and improve well-being. But, they might cause side effects like mood changes or weight gain.
Surgical Treatments
If nonsurgical treatments don’t work, surgery might be needed. Laparoscopic Surgery is a minimally invasive method. It lets doctors see and remove endometriosis lesions. This surgery is also key for diagnosing endometriosis.
If laparoscopy doesn’t help enough, a hysterectomy might be talked about. This is especially true for those who don’t want to keep their fertility.
It’s important to remember that surgery can help symptoms but might not stop them from coming back. This means ongoing medical care is still needed.
| Treatment Type | Description | Typical Outcomes |
|---|---|---|
| Nonsurgical | Medications like NSAIDs and Hormone Therapy. | Reduction in pain and improved quality of life. |
| Surgical | Laparoscopic Surgery for lesion removal. | Potential elimination of lesions and symptom relief. |
| Hysterectomy | Removal of the uterus, often discussed when fertility is not a priority. | May provide substantial symptom relief, but not guaranteed. |
Finding the right mix of treatments depends on many factors. This shows why a personalized care plan is so important for managing endometriosis well.
Living with Endometriosis: Coping Strategies
Living with endometriosis is tough, but there are ways to cope. Joining Support Groups is a big help. Here, people share their stories and learn from each other. It’s a place to find comfort and feel less alone.
Making lifestyle changes can also help. Eating well and staying active can reduce pain. Try to exercise for 20 to 30 minutes daily. It boosts mood and fights inflammation.
Stress management is key too. Mindfulness and yoga can help handle stress. This can lessen the pain caused by stress.
Don’t forget about mental health. Medicare can help pay for mental health services. This includes talking to psychologists and other health experts. Also, seeing a pelvic floor physiotherapist can help with pain without needing a doctor’s note.
Keeping in touch with your healthcare team is important. Regular check-ups and adjusting treatment plans are vital. A mix of medical care, support, and lifestyle changes can make a big difference in your life.
Conclusion
Endometriosis awareness is key for those dealing with this complex issue. It often takes 7 to 9 years to get a correct diagnosis. Knowing the symptoms and risk factors like early menstruation and heavy bleeding is crucial for seeking medical help early.
Understanding endometriosis helps people manage their health better. They can look into treatment options and find the right care. This knowledge empowers them to take charge of their health.
Research is ongoing to tackle the challenges of endometriosis, especially its effects on fertility and well-being. While there’s no cure yet, treatments like pain relief medications and hormonal therapies can help. Even simple changes in diet may ease the pain.
Boosting awareness and supporting research can lead to better treatments and a better life for many. Education and understanding are vital. They help those affected navigate the challenges of endometriosis and work towards better health.
FAQ
What is endometriosis?
Endometriosis is a condition where tissue like the uterus lining grows outside the uterus. It often causes pelvic pain, heavy bleeding, and infertility.
What causes endometriosis?
The exact cause is still unknown. But, it might be linked to menstruation going backward, genetics, immune issues, and hormones, especially estrogen.
What are the common symptoms of endometriosis?
Symptoms include severe pelvic pain, painful menstrual cramps, and heavy bleeding. Other signs are pain during sex, infertility, and stomach problems like bloating and constipation.
How is endometriosis diagnosed?
Doctors start with a detailed talk about symptoms and a pelvic exam. They might use ultrasounds or MRIs. Sometimes, a laparoscopy is needed to confirm the condition.
What risk factors are associated with endometriosis?
Risk factors include a family history of endometriosis, early menstruation, shorter cycles, and never having given birth.
What complications can arise from endometriosis?
Complications include infertility, chronic pain, and problems with bowel or bladder function if tissue grows near these areas.
What are the treatment options for endometriosis?
Treatments include pain relief with NSAIDs and hormone therapy. Surgery like laparoscopy is also an option, especially for severe cases.
How can individuals live well with endometriosis?
To cope, join support groups, make lifestyle changes, manage stress, and talk openly with healthcare providers.